Treatment Options for a Herniated Disc (Non-surgical and Surgery)
If you are suffering from lower back pain and sciatica which is the result of a herniated disc, surgical treatment may be an option. Dr.Likover has helped many people relieve pain by conducting successful non-surgical and surgical treatment. Schedule a consultation and learn your treatment options.
Table of Contents
- What is a herniated disc?
- What causes pain from a herniated disc?
- How does a herniated disc typically happen?
- How is a herniated disc diagnosed?
- Nerve Exams
- Surgical Herniated Disc Treatment
- Non-Surgical herniated disc treatment
- Common questions about herniated discs
What is a herniated disc?
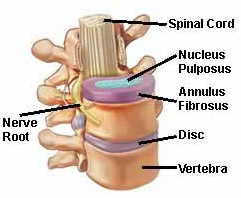
A herniated lumbar disc refers to an issue involving one of the rubbery pads, or discs, that lie in between the individual bones (vertebrae). A disc herniation involves an injury to the pad, or disc, which sits in between the lumbar vertebral bones.
What causes pain from a herniated disc?
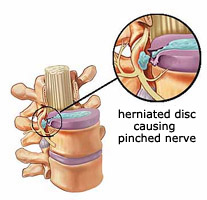
The cause of pain from a herniated disc is that the herniated disc puts pressure on one of the lumbar nerves which causes inflammation which the brain perceives as pain, numbness, tingling, or weakness that is felt in the leg as a “sciatica” syndrome. The goal of treatment is to alleviate pressure on the nerve, which causes the leg symptoms. A few individuals have a “central” disc herniation, which causes only back pain without any significant leg pain.
How does a herniated disc typically happen?
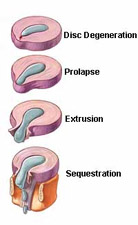
The spinal disk has a soft, jellylike interior referred to as (the nucleus) that is contained in a tougher exterior called the (annulus). A herniated disc occurs when the nucleus breaks through the annulus. Essentially, a herniated disc can occur in any part of the spine and may cause some numbness, pain, and weakness to the leg or arm depending on the affected area. Herniated discs commonly occur in the lower back (lumbar spine) and in the neck (cervical spine). The most reported incidents in which a herniated lumbar disc can occur include lifting heavy objects, twisting, falling, sneezing or another type of injury. However, some individuals also do not report any specific, unique incident that led to the rupture of a disc.
Who is more at risk to get a herniated disc?
Often a herniated disc is the result of the gradual wear and tear of aging (disc degeneration). This makes older people more at risk for this type of injury and men are twice more likely than women to be affected. Other factors include:
- Being overweight
- Lifting heavy objects repeatedly
- Sitting position for a long time
- Repetitive twisting and bending (sports, work and etc)
- Smoking
How is a herniated disc diagnosed?
In most cases, a herniated disc can be detected by your doctor with a physical exam and examination of medical history. During your physical exam, the doctor will examine the following:
- Muscle strength
- Reflexes
- Ability to walk
- Ability to feel light touches
- Series of stretches
In some cases, your doctor may order an imaging test to rule out any other conditions.
Imaging Tests
X-rays
Despite x-rays not being able to detect herniated disc’s this test is requested simply to rule out other causes such as spinal malalignment, a tumor, a broken bone, or an infection.
Computed tomography (CT Scan)
A CT scan examines a series of x-rays from various angles and combines them in order to examine sections of the spinal column.
Magnetic Resonance Imaging (MRI)
This type of imaging uses radio waves and a strong magnetic field to create images of the internal structure of the body. Doctors will often order this examination to confirm the precise location of the herniated disc and to see which nerves are affected.
Myelogram
During this procedure, a dye is injected into the spinal fluid before x-rays are conducted. This test allows doctors to see any pressure on your spinal cord and nerves due to multiple herniated discs.
Nerve exams
Electromyogram (EMG)
During this exam, your doctor will insert a needle electrode through the skin in various muscles. This test evaluates how the muscle responds to the electrical activity when at rest and during contraction.
Nerve conduction study
This exam observes the muscle and nerve impulses with electrodes placed in the skin.
Herniated Disc Treatment
Non-Surgical Disc Treatment
CONSERVATIVE TREATMENT: The conservative treatment for a disc herniation consists of as much rest of the back as possible. One should certainly avoid all types of strenuous sports and work activities. I recommend strict bed rest for several days only if the person is in extreme pain. I usually prescribe pain medication, anti-inflammatory medication, and muscle relaxants if muscle spasm is a major component of the individual’s case; however, if symptoms persist an epidural steroid (injection deep in the back) may be recommended. Generally, the patient is given six to eight weeks to get over his or her problem with rest, time, and conservative treatment. It is well documented in the orthopedic literature that a fairly significant percentage of people will get over an acute lumbar disc herniation with time. The reason this happens is that the herniated disc shrinks down and ceases to put pressure on the nerve to the leg. If this occurs, the individual gradually gets better. Up to fifty percent of people will get over a lumbar disc herniation without surgical treatment.

Surgical Disc Treatment
SURGICAL TREATMENT: An individual, who fails conservative treatment and continues to have pain or foot weakness for a significant period of time, is a candidate for surgical correction of his herniated disc. The level or herniation in the lumbar spine and the pattern of herniation are usually determined initially by a magnetic resonance imaging study (MRI) or a computerized axial tomography (CAT scan) with lumbar myelogram. A MRI is now considered to be the first test done in most cases because it is an outpatient test, which is noninvasive, and there is no requirement for radiation. MRI can diagnose approximately 90% of herniated discs. A small percentage of herniations are missed by an MRI. For this reason, it is sometimes necessary to do a myelogram-CAT scan to make the diagnosis. A myelogram involves dye being placed within the spinal fluid so that an x-ray showing the nerves can be taken. Also, in certain cases, for surgical technical reasons, a myelogram is necessary before surgery.
Upon determination of the type of disc herniation the most appropriate type of surgical procedure is then recommended by me.
There are two types of lumbar laminectomies for people who have a herniated lumbar disc requiring surgery to correct their problem.
TRADITIONAL LAMINECTOMY: A traditional lumbar laminectomy usually requires a three to four inch incision in the center of the back and the herniated lumbar disc is removed from under the nerve root. Once the pressure is removed from the nerve root, the individual gets well. A traditional laminectomy requires hospitalization for three to four days. The individual generally returns to light work at two to four weeks and heavy work at three to six months.
MICRO-LAMINECTOMY: A newer and preferred way of doing a lumbar laminectomy has been developed in the last few years. Micro-laminectomy accomplishes the same goal as traditional laminectomy. The herniated disc is still removed from underneath the nerve root and nerve pressure is alleviated such that the individual’s symptoms are relieved. The difference between a micro-laminectomy and traditional laminectomy is the size of the incision and the muscle separation required. A micro-laminectomy on a thin individual can usually be accomplished with a 1-inch to 1.5-inch incision. New microsurgical instruments have been developed to allow for this type of surgery with a small incision. Not only is the skin incision small, but the incision in the muscle is small, thus minimizing the injury to the low back muscles and ligaments. Only one level of lumbar spine structure is exposed for a one level herniation. If two herniations are present, then only the two lumbar spine levels that are involved are exposed.
The fact that only a very small incision is made in the back area makes for a much quicker recovery time. Most people are up walking on the day of surgery and are back to light work, i.e., office work within three to seven days. Micro-laminectomy is done as an outpatient procedure. With micro-laminectomy, people generally get over surgery much quicker. For example; I have had several runners return to jogging at four to six weeks following their surgery.
The success rate for micro-laminectomy and traditional laminectomy are the same. Generally, the success rate for one level herniation is over 95% in obtaining relief of most leg pain and associated symptoms. It is felt that the small percentage of individuals who do not improve substantially following micro-laminectomy have nerve damage that was present prior to surgery due to pressure on the nerve. It is impossible to diagnose whether permanent nerve damage is present prior to surgery. Curing a postoperative persistent pain syndrome after a failed laminectomy is a major unsolved problem in orthopedics. Persistent pain or numbness in the hip and leg following micro-laminectomy is one reason orthopedists do not like individuals to go on for a prolonged period of time before having surgery with substantial pressure on their nerve root, as most orthopedists believe that there is a possibility of significant irreversible nerve damage occurring in the nerve root.
Currently there is no good replacement for the disc that is removed; the individual lives without it. Most people do well despite missing only a portion of the lumbar disc as only the central portion of the disc, the nucleus, is herniated and surgically removed. The remainder of the disc, the annulus, remains in place so that the adjacent bones do not touch or come together. Some people do not have periodic backache or leg ache. Most people are cured of the leg pain and are much better off than they were prior to surgery because of the absence of pressure on their nerve.
Micro-laminectomy is the safest and best way for a person suffering from a herniated disk to obtain relief of their pain symptoms due to a lumbar disc herniation. Postoperative pain is substantially less and recovery is dramatically quicker than with traditional lumbar laminectomy.
If you have questions, I will be happy to answer them. Contact me by clicking here to send me a message or call me at 713-465-0696.
Larry L. Likover, M.D., P.A.
FAQ
Is a herniated disc curable?
Usually, a herniated disc will cure over time. It will largely depend on how affected the area is, rest and if surgery is needed. However, Dr.Likover can properly asses the area to give you a few options to get it cured.
Can a herniated disc heal on its own?
In some cases, a herniated disc will cure on its own. This will depend on taking care of the affected area by stopping a certain exercise that makes pain worse, proper diet and how affected is the area.
When is a herniated disc serious?
In general, if a herniated disc causes changes in bowel or bladder, loss of feeling in arms or feet its recommended you go see a doctor immediately.
Can herniated discs cause sciatica?
Yes, when a herniated disc pushes against a nerve in the lumbar spine this may travel through the leg or foot causing sciatica.
 Dr. Larry Likover has been practicing orthopedics on the west side of Houston for 43 years, treating knee, hip, shoulder, and back problems. Dr. Likover is board certified in orthopedic surgery and provides knee replacement in Houston for patients worldwide.
Dr. Larry Likover has been practicing orthopedics on the west side of Houston for 43 years, treating knee, hip, shoulder, and back problems. Dr. Likover is board certified in orthopedic surgery and provides knee replacement in Houston for patients worldwide.